A teenager’s dreams would take a different turn; her career aspirations would be replaced with the hope of recovery. She would not find it in Kosovo.
Luljeta Lubovci, now 28, was injured at the age of 15 while going to school on a particularly cold winter day.
“I slipped on ice and fell on my back… I had intense pains. My parents took me to the neighborhood’s ambulance,” she recalls. “There, they told me that it would be better if I saw an orthopedist, and in the afternoon, I went to a private orthopedist for examinations and he said, “I can’t do anything for you. You need to see a neurosurgeon.”
It was 2007 — Kosovo had not yet declared independence. State institutions at the time were called provisional and self-governing and operated under UNMIK regulations. Although there was an independent health system, it was still unconsolidated, and there was a lack of medical experts in some fields in the regional hospitals.
Lubovci noticed these absences in the regional hospital of Prizren where she was being treated. “Once a week at that time two private neurosurgeons came and I went [to the hospital where one of them] gave me medication and physical therapy, but the condition did not improve even after about six months of therapy,” she says.
At one point she was forced to undergo surgery, but the problem was still not solved.
“We thought about it for a few days, and we decided that I would undergo surgery with [a doctor at a private hospital] for a herniated disc. He did the surgery, but I was still not OK, I did not see any difference,” she says. “After two months of therapy and rest, and after yet another examination, they told me I needed to urgently undergo surgery yet again — no later than the next day. My family was forced to accept the surgery. Afterward my condition kept on worsening.”
Today, 13 years later, just like Luljeta, Anita* also has walking difficulties. Her condition is deteriorating while she is on the waiting list for surgery at the University Clinical Center of Kosovo. As she waits, she is not allowed to be treated in private institutions or abroad.
For treatments that are not performed in state institutions, be it in the country or abroad, Kosovo has a Program for Medical Treatment Outside of Public Healthcare Institutions. The program operates within the Health Insurance Fund (HIF) that has been operational since 2018, four years after the adoption of the Law on Health Insurance.
Those who are granted access to this fund are reimbursed 70% of the funds needed for treatment. For cases considered emergencies, the procedures are expedited, while for others a considerable number of documents are needed to apply.
In order to secure the money they did not have, members of her family took out loans.
Luljeta and others in need of medical treatment abroad could benefit from an agreement reached in 2009 between the health ministries of Kosovo and Turkey, which aims to provide patients with treatment for health services that are not offered in the country. According to the agreement, the selection of patients must be done by the Ministry of Health in Kosovo and approved by the one in Turkey, while the responsibility of Kosovo institutions is only to provide travel tickets for patients and their companions.
The agreement, which stipulated the free treatment of 100 patients in Turkish hospitals within a year, has rarely been fully implemented.
Knocking on door after door
Now, Luljeta claims that her second surgery had errors that caused long-term consequences that she still faces today. “The situation worsened; after a while, I was told to go to Turkey for another surgery and therapy, but it cost 20,000 euros, and my family had already spent a lot of money on me,” she says.
In order to secure the money they did not have, members of her family took out loans.
“Anyway, they somehow collected [the funds] with a loan and I went and had the surgery,” she recalls. “I had a very difficult 13-hour operation — they put screws and plates on my back. I stayed there for about 10 days; I felt better, but it did not last long [and] I still had to have surgery in Kosovo with Dr. Haxhi Avdyli.” This neurosurgeon, according to her, instructed her to seek treatment abroad.
“Some friends also looked at French hospitals; they said that the operation alone costs around 40,000 euros, plus the rest, the hospital… My family and I no longer had [the funds] because we had spent a lot.”

Although Kosovo has an agreement that allows patients to get treatment in Turkey, citizens often follow this route privately. Photo: Saranda Ramaj / K2.0.
A few years later, Luljeta says that she and her family saw the Ministry of Health as an opportunity to get help for her. “I thought I’d try it with the ministry. I went, applied, and submitted the necessary documents. I was told that they would ‘notify me when the commission makes [a decision]’. I waited, but I did not receive an answer,” she recalls.
She even says that she knocked on the door of the then Minister of Health, Ferid Agani.
“He welcomed me; we talked for quite some time. He said, ‘We do not have enough budget, I have to wait in line; even if we manage to, we can only cover half’. At some point I told him: ‘Minister, since you don’t have money, can you help me get a visa for France? He said, ‘Let’s see, we will let you know, we will talk’, and they never got back to me,” she continues.
According to the Administrative instruction on medical treatments outside the public health institutions, institutions cannot help provide visas for patients whose treatment is not approved. K2.0 has contacted Agani but did not receive an answer before the publication of this article.
Meanwhile, Luljeta’s pain only increased as days went by. Although she was young, she used strong morphine-type analgesics to alleviate it.
“My condition was getting worse, I was getting very tired, and I was bed-bound,” she painfully recalls. “They would give me four shots of intramuscular morphine and I would spend 20 euros a day on needles, but those drugs would make me dizzy, I would lose consciousness.”
But the medicine was not meant to cure her — they only helped her cope with the difficult reality she lived in. Just hours after she was injected with morphine, the pain would return.
Without a response from the Ministry of Health, the only solution left for her and her family was to accept that her case be made public and to collect money from good samaritans. Fundraising campaigns for those in need of treatment abroad are numerous and frequent — they range from posts on social media and collecting money from people on public squares to the involvement of celebrities to help.
Even after the money was raised, it was still a bumpy road ahead for Luljeta.
“For about a month they asked [for money] at the university where I was studying; they asked friends and other people, various activities took place,” she says. “Some 25,000 euros were raised.”
“However, my visa was denied by the Swiss Embassy twice in a row.”
Crossing borders in search of health
Luljeta’s efforts towards recovery are not over yet, but she no longer has any hope in Kosovo’s public health system. In the absence of help from her birth country’s health institutions, she has long since left.
She is continuing her life away from her family and with an unusual daily routine for people her age: she does therapy as soon as she wakes up and finishes by the time she has to go to sleep. Sometimes she says that even the medicine does not work, even though sedatives’ doses have increased over the years.
She “escaped” for recovery five years ago — she says she has found hope in France.

Luljeta Lubovci, who was studying international management, left Kosovo during her last years of studies. Photo by Luljeta Lubovci.
Searching for a remedy, she had taken illegal routes to cross borders during the winter.
From France, where she still receives health services, she recounts her efforts to recover. “My family found someone illegally that would help me get to France — my father was accompanying me. They asked for 6,000 euros for the both of us,” she said, five years after crossing the borders of five countries to arrive in France.
She remembers that cold and rainy February night in detail. The illegal crossing was not easy, and the illness made her journey even more difficult. She explains that she was forced to do part of the journey on foot, a task that is not easy in her condition.
“We passed through Serbia, Hungary, Austria, Germany, France,” she recalls, saying that the most difficult part was illegally crossing from Serbia to Hungary. “It took us 15 minutes to cross the border on foot. I could not walk much, but my father and a gentleman from Deçan, who we met in Serbia, helped me.”
They had somehow made it to France, but her condition had worsened even further.
“After much difficulty, fear, pain, I went to an ER. There, I was thankfully taken in and was hospitalized for three weeks in the French city of Annecy,” she says.
But the rare disease that she had been diagnosed with could not be treated in that city, so she had to go about 800 kilometers away to the city of Toulouse.
So far, she has undergone four operations in France.
“After the treatment, the doctors said, ‘We will operate on you, but your treatment will last for years, you have to stay here,'” she recalls, adding that the hospital staff there provided her with temporary accommodation, assisting her with all the necessary paperwork to get health insurance.
After the hardships she went through over the years, while waiting to undergo yet another surgery in France, she says that she now receives good health services.
Loan-fueled health care
Parents have also been trying for a long time to get medical services for their children. Rashit Gashi from Prishtina, since the birth of his son seven years ago, has been wandering around the health institutions of Kosovo to get a correct diagnosis for his son. It has already been confirmed that Rashit’s son has an autism spectrum disorder as well as Attention Deficit Hyperactivity Disorder (ADHD).
Facing the need for treatment abroad, Rashiti says that he and his family have done it all alone. He says the treatment has become more difficult in the last four years, as has the financial burden. “It’s about 22,000 euros that I have spent in the last four years,” he says.
He is currently unemployed. In the past, he was employed and a strong unionist voice in the Electricity Distribution Company in Kosovo (KEDS) where his contract was terminated not long ago.
Left without any income, he still has to find a way to provide genetic testing for his son. He describes this type of test as a method to explore brain development issues in his son. It is not performed in Kosovo’s public healthcare institutions but is offered abroad and in private institutions within the nation.
But the cost is overwhelming for the family, so Rashiti says that they decided to seek help from the Program for Medical Treatment Outside of Public Healthcare Institutions that operates within the FSSh.
To be eligible to apply for this fund, a collegium of three doctors must sign a document proving that the treatment the patient needs cannot be done in public hospitals.
But Rashit's difficulties are not just about the means to do medical tests.
Rashiti says that when he delivered the signed document to the FSSh officials, they did not accept it. “This is not a report,” he recounts them saying. “They gave me a consultative opinion saying ‘[the patient] is instructed [to receive] multidisciplinary treatment.’”
He went back to the University Hospital and Clinical Service of Kosovo to receive a new report. There is little hope that this time the aid will be approved. “One of the FSSh workers told me, ‘take an application, but we have never approved such requests.'”
He also sent two pro forma invoices for the analysis, as legally prescribed. One of the pro formas is in Olive laboratory in Kosovo, the other in a hospital in Macedonia. “The laboratory pro forma in Kosovo costs 1,800 euros, while in Macedonia it costs 2,500 euros. The Kosovo laboratory does not do it itself, but only takes the sample, sends it to Turkey, and then returns the result,” he explains.
But Rashit’s difficulties are not just about the means to do medical tests. It has been more than a month since his seven-year-old son has started requiring special food, and the financial burden for these expenses is not covered by the state at all.
“It is the fourth week since he has started [using] special food, with fiber, food made out of pine seeds that I didn’t even know existed; it costs 85 euros per kilogram,” he says. “The costs are 400 euros a month only for food.”
This figure increases when including the other services he has to pay for, such as the boy’s caregiver. In the absence of state aid, Rashiti has been in debt for years. Unemployment has already made it difficult for him to repay the loan.
“All these years we have covered the expenses only with loans because in the beginning, it was not that we had a lot of relatives and family members; we kept this issue a semi-secret, so we had to deal with it ourselves,” he says. “Since my employment contract was terminated, my friends are helping me.”

The case with their seven-year old is not the first time the Gashi family has sought help from the Health Insurance Fund. Photo: Saranda Ramaj / K2.0.
The Gashi family’s struggle with financial costs for health services not provided in Kosovo goes back even further to when Rashit’s father was diagnosed with cancer seven years ago. The University Clinical Center (QKUK) had told him that at that stage, he could only be offered chemotherapy, but a second opinion in a country in the region had recommended that he be operated on.
They could not apply for funding from the Fund because they could not obtain a consultative opinion that would allow him to be treated abroad.
“They said that he is at a late stage and that nothing could be done; in the absence of the report we did not manage to apply for this fund,” he recalls and shows that he had sent his father for treatment to Albania, where was operated on in a private hospital. “The operation cost around 7,700 euros.”
A year and a half later, the patient had passed away.
Waiting for the state
For a long time, Anita has also been waiting for state-help to improve her health. Her life has changed radically for the worse, especially in the last three years when her movement has been restricted.
Her husband has often gone to the QKUK these past few years to ask when his wife will be able to undergo surgery after being included on the waiting list for orthopedic surgery three years ago.
“On December 7, 2017 we went for a check-up. We were told that there is a waiting list and we must be registered. My wife was added to the list. She was the 154th patient or something like that,” he says.
He thought that their turn would come by now, but no one has called him from the QKUK yet. Meanwhile, his wife’s condition has worsened, and she can only move very short distances. “She can walk about 20-25 meters, no more,” he says.
No one in their family works, and their financial situation is dire.
Orthopedic surgery costs about 10,000 euros. According to Anita’s husband, the operation she is waiting for is offered in many private clinics, but they cannot afford it. The only solution is to wait their turn on the list that the QKUK should be using to carry out the operations.
Surprisingly, three years later, he says that his wife’s name has gone even further down the list, while patients who have appeared later have been selected to have surgery earlier. “When I went this year to see why she was not called, the hospital told me she was 174th on the list — I was surprised [because] she was 154th three years ago,” he said.
He says that the doctors have warned him that if there is not an intervention in time, she risks being immobilized.
The fact that the waiting lists at the Orthopedic Clinic at QKUK date back to 2017 is evidenced by the institution’s official data. It talks especially about three services that patients are still waiting for 3 years later: hip prostheses, knee prostheses and for ligament surgery.
The longest list is that of patients waiting for knee prostheses. “There are 106 people on the 2017 waiting list, 306 in 2018, 303 in 2019, 91 in 2020,” the data confirms. There are a total of 806 patients waiting to receive this treatment. The queue for surgery is also quite long; there are currently about 700 people on the waiting list.
Anita’s husband explains her pain as unbearable. He says that the doctors have warned him that if there is not an intervention in time, she risks being immobilized.
He says that he tried to get help from the FSSh, but he was immediately rejected, according to him. “When I went there, I was told ‘no because QKUK provides this service, and we only cover services that are not provided in hospitals,'” he says.
Help denied
Besim Kodra has been leading the Association for the Protection of Patient Rights in Kosovo for several years. This organization receives many complaints about health services, but according to Kodra, there are frequent cases when complaints are made about the lack of opportunity to be cured, even when diseases are treated in Kosovo.
“This fund [for treatment abroad or outside public institutions] is discriminatory in its content as it supports diseases that are not treated in public institutions, while patients who can be treated in public institutions despite the long and unreasonable wait due to absences in the supply of consumables and medicines, are not supported by the fund,” he said. “This has held up the lives of some citizens for long and unreasonable periods of time.”
“We have received frequent complaints from patients who are not supported by this fund after the QKUK issued a certificate in which it wrote: ‘This intervention is not performed in the QKUK, but if we had consumables and drugs we would do treatment’. Such certificates were not accepted by the FSSh and thus the patient could not get support from the Fund nor could they be treated at the QKUK,” he explains.

The leader of the Association for the Protection of Patient Rights Besim Kodra says that patients are denied treatment due to the lack of consumable materials in public institutions. Photo: Besim Kodra.
When these patients and other patients were facing unresolved health problems, the state was able to send some of them to Turkey for treatment without spending any money. For a decade, the Ministry of Health has never fully implemented the agreement with the Turkish state.
Travel tickets were the only expenses to be paid by the Government of Kosovo as set out in Article 5 of this Agreement, a copy of which has been obtained by K2.0.
“Pala turke duhet të ofrojë trajtim në spitalet e Turqisë për 100 pacientë nga Kosova që nuk mund të trajtohen në spitalet e Kosovës”, thuhet në paragrafin e parë të marrëveshjes.
“The Turkish side must provide treatment in Turkish hospitals for 100 patients from Kosovo who cannot be treated in Kosovo hospitals,” reads the first paragraph of the agreement.
While the MoH did not utilize this agreement, it spent large sums of money to pay for services for the same category but outside the agreement. From the partial documents obtained in 2013, the MoH has paid more than 1 million euros to hospitals in Turkey.
For nine patients, Acibadem Hospital alone was paid about 125,000 euros, and the other Turkish hospital, Isil Halgig Hymzet, was paid around 150,000 euros for the same number of patients. From the data provided from 2013, these hospitals are mostly contracted by the Ministry of Health and this is also confirmed in the annual report of the Health Insurance Fund for 2019. It states that for the first time last year, the responsible institutions have fully used the agreement.
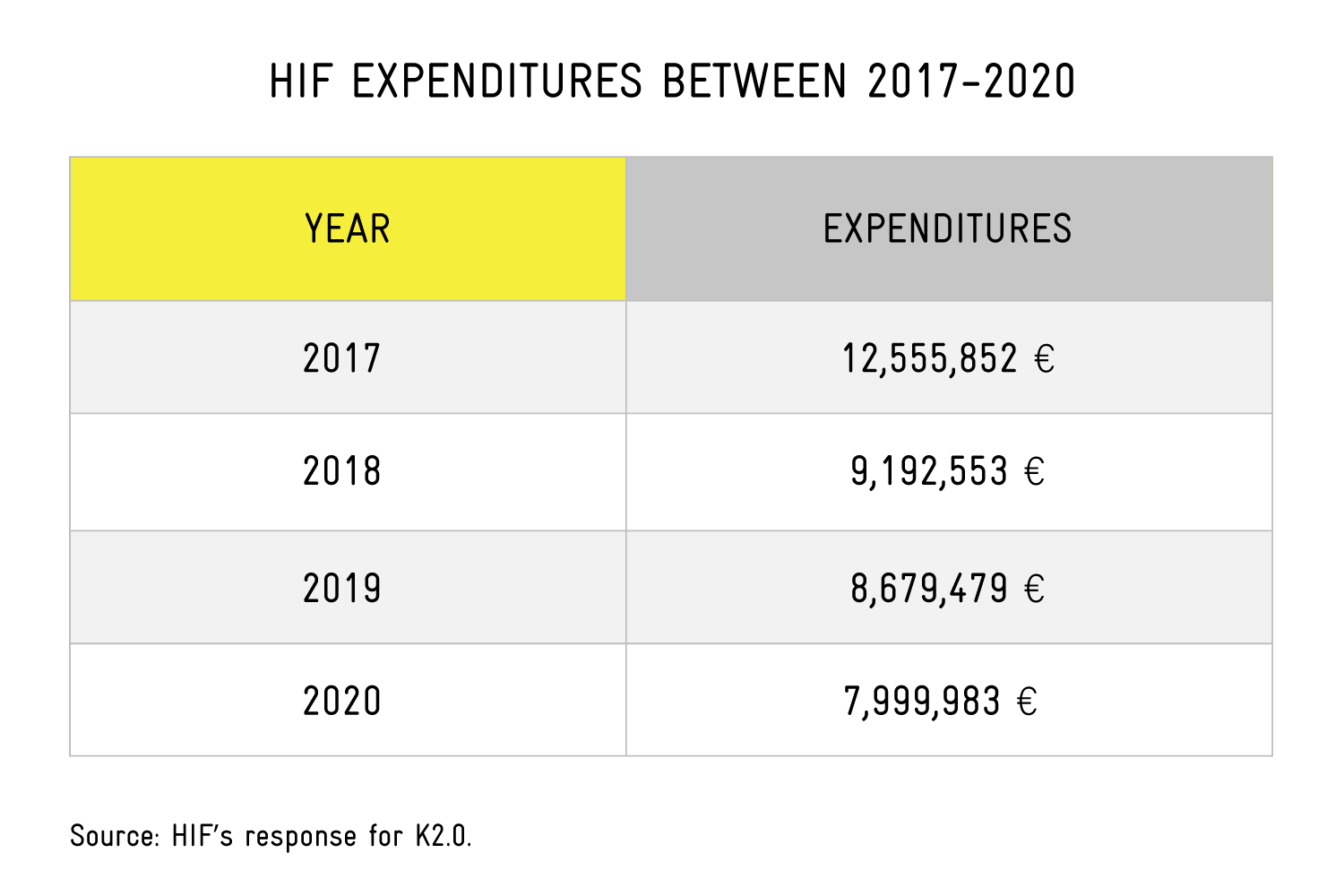
Out of about 1,400 patients who sought help in 2019 from this institution, about 130 of them were rejected. While in 2020, according to the director of the Health Insurance Fund, Fatmir Plakiqi, there were fewer requests than in previous years. “The number of applications/requests until [August 2020] is 918,” he said.
There are some areas for which there are more requests for treatment abroad, he told K2.0: “The clinics that refer patients the most are: Pediatrics (pediatric heart surgery; leukemia and other malignant diseases, etc.,) Ophthalmology, Orthopedics, Hematology (malignant diseases in adults.)”
Plakiqi has denied that there is institutional bureaucracy in reviewing requests for treatment abroad. He says that the procedure is performed within a week for urgent cases and for those who can wait within two weeks.
“Regarding the decision-making procedures for elective cases (non-urgent)… the commission of the Ministry of Health lasts approximately for one week from the moment of application, while until the approval of the financial amount (for elective cases) by the Executive Board … the duration is approximately two weeks,” he said. “Meanwhile, for emergencies… FSSh issues a receipt/guarantee within the day or at the latest the next day, which means that the patient can start the necessary health treatment immediately.”
At least 20 patients’ rights were violated when applying for treatment outside public institutions in 2018; The MoH lost 20 court cases against disgruntled patients that year. From these court decisions, the institution has been forced to pay about 115,000 euros.
In 2019, the right through the court against the FSSH was won by six citizens.
According to the administrative instruction for medical treatment outside public health institutions, the state must cover the costs for services not provided in the public health system, and the possibility of treatment in private health institutions is not excluded.
This administrative instruction was last amended in 2017. It stipulates that a patient within a year cannot be paid more than 30,000 euros; exceptions are persons under 18 years of age and social cases.
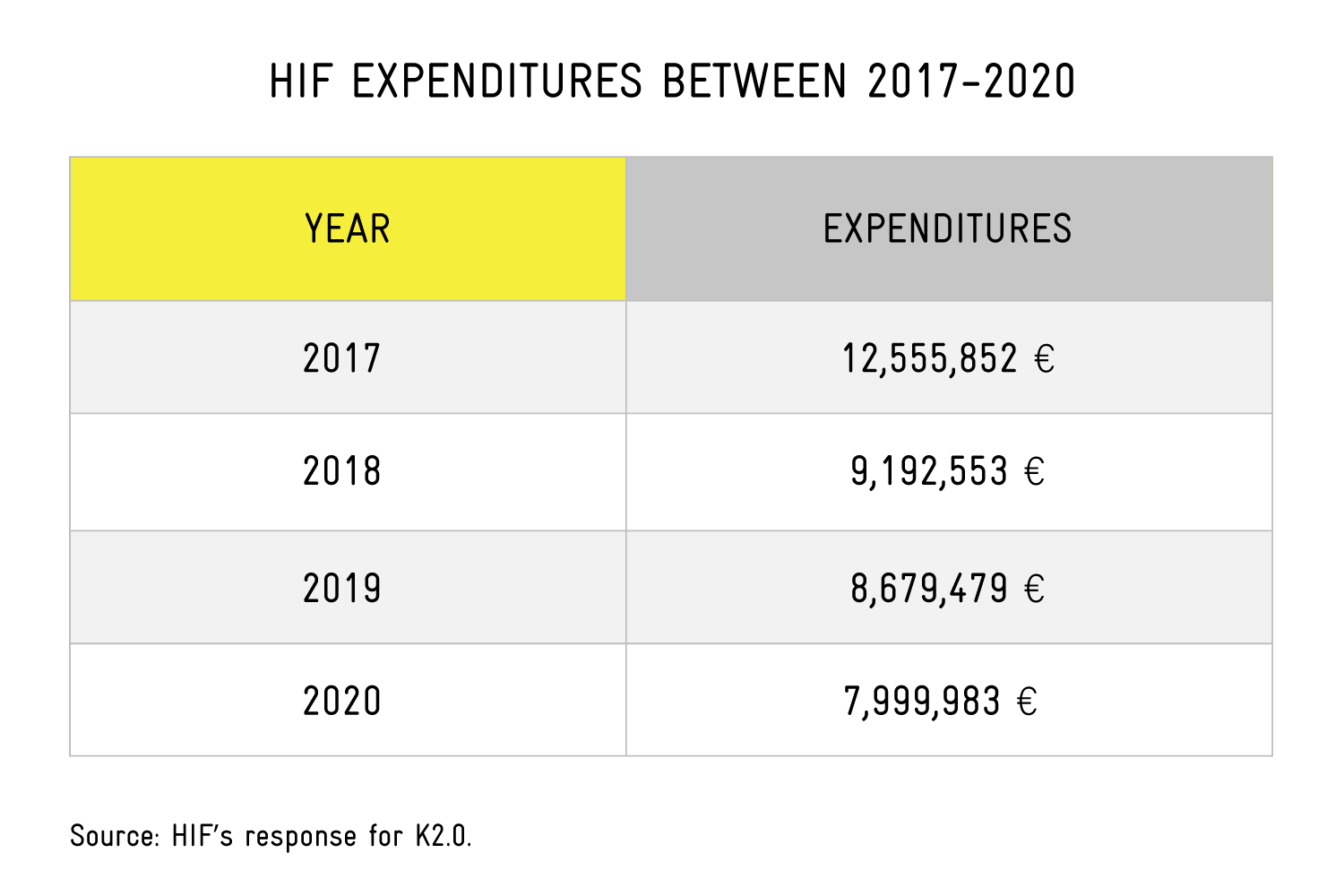
The FSSH owes several million euros to several hospitals. “Outstanding liabilities until November [2020], are: 5,936,802.85 [euros],” told director of FSSh Plakiqi to K2.0.
According to Besim Kodra from the Patient Association, this lays bare the dysfunction of the health system.
“[The program] for treatment outside of public health Institutions has been and remains a major problem both in its conception and in the way it works,” he says. “This fund [FSSh] is constantly overloaded with patient requests for financing, as a result of the normal non-functioning of health institutions in the Republic of Kosovo.”
According to him, this way of functioning has influenced the FSSh to get into debt, “although with the Law on Health Insurance, such a thing is prohibited as it is says that the Fund neither borrows or lends.”
According to the documents obtained by K2.0, most of the FSSh budget has gone to cases of heart disease that were not performed in the public system until 2019. At the inauguration of the renovation of the Invasive Cardiology Unit at QKUK in 2019, former Minister of Health Uran Ismaili said that “the impoverishment of citizens in search of a health service [was coming to an end].” However, this did not happen; even after the invasive cardiology services started in the state hospitals, the annual expenses have not been reduced, according to official data.
Even one of the biggest corruption scandals in terms of the severity of financial damage and the number of defendants, known as the “heart crime” or the “Stenta” scandal, is related to cases at a time when invasive cardiology services were not provided in state hospitals.
For such an affair, made public in 2014, an indictment was filed against former Minister of Health Ferid Agani, and 60 officials and doctors accused of sending patients from public hospitals to their colleagues in private hospitals. In April 2019, the Basic Court in Prishtina sentenced former Minister Agani to two years and six months in prison for abuse of office. At the end of 2019, his case was returned for retrial by the Court of Appeals.
If the Program for Treatment Outside Public Health Institutions worked adequately, and the agreement with Turkey to send 100 patients from Kosovo for free treatment was fully implemented every year, perhaps Luljeta Lubovci would not have to go through five countries illegally to seek treatment in France.
Even the husband who has been waiting for three years now for his wife Anita to be treated at the QKUK would not ask the desperate question: “Do I have to die to get a service or what?”
*Anita is a pseudonym to protect the identity of the person in question.
Feature image: Saranda Ramaj / K2.0.
This publication is part of the third cycle of the Human Rights Journalism Fellowship Program, supported by the European Union Office in Kosovo. The program is co-supported by the National Endowment for Democracy. This program is being implemented by Kosovo 2.0, in partnership with Kosovar Center for Gender Studies (KCGS), and Center for Equality and Liberty (CEL). Its contents are the sole responsibility of Kosovo 2.0 and do not necessarily reflect the views of the donors.